Hamstring Rehab: Balancing functional progression and underlying deficits
Available in:
EN
Simon Harries is the Manager of Physical Preparation at the NSW Institute of Sport. With more than 15 years of experience as a Strength & Conditioning (S&C) coach and rehab specialist across the Australian Football League (AFL), Rugby League, Rugby Union, Rugby Sevens, water polo and a range of individual event sports, he is focused on supporting S&C coaches and physiologists to deliver world-class performance support to their elite athletes. He is also the Founder of Performance Compass, where he supports rehab practitioners in navigating the complexities of rehab environments.
In this article, Simon discusses why assessments matter and why context is just as important. He outlines the complexities of hamstring rehab in an anterior cruciate ligament (ACL) injury case he managed, highlighting why functional progress alone is not enough and how tools like the NordBord and ForceDecks can help identify hidden deficits that impact return-to-play readiness.
Rehab is Murky
Hamstring rehab exists in a space where the restoration of function does not always equate to the restoration of underpinning capacities. This became evident in a highly recurrent hamstring strain case involving an ex-professional rugby sevens player who now competes at the sub-elite level.
Hamstring rehab exists in a space where the restoration of function does not always equate to the restoration of underpinning capacities.
The athlete sustained a significant hamstring strain injury. No medical imaging was performed, but it presented as a likely grade 2 distal biceps femoris strain. His rehab was managed by an experienced and capable team, but as is often the case in sub-elite environments, they lacked the resources and technology to support objective decision-making. Seeking further insights, the athlete approached me for a second opinion.

At eight weeks post-injury, he had returned to sprinting at 88% of his max velocity and was also performing change-of-direction drills and sport-specific skills. However, he remained hesitant when accelerating and running beyond 80% max speed. On the surface, his function had returned, but hamstring strength testing painted a different picture:
|
Athlete Performance
|
Athlete Asymmetry
|
Benchmarked Standard
| ||
 | Nordic Hamstring Exercise |
Affected: 2.8N/kg
Unaffected: 4.15N/kg |
32.5%
|
4.4N/kg (50th Percentile)
|
 |
Hip
Iso-Push |
Affected: 1.2x SW
Unaffected: 1.7x SW |
29.4%
|
2-2.5x SW
|
|
SW: System Weight
N: Newton
kg: Kilogram
|
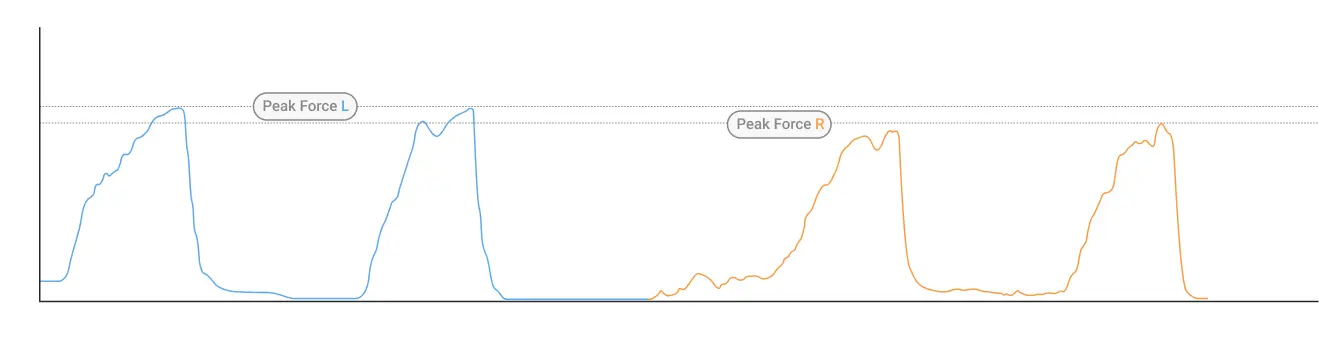
- 32.5% asymmetry in eccentric hamstring peak force (Nordic Hamstring Exercise), with absolute values well below expected Norms (<2.8N/kg injured side vs. 4.15N/kg uninjured side). According to the VALD 2021 Normative Data Report from Rugby Union, these values placed the athlete in the 10th percentile for the injured limb and 40th percentile for the uninjured limb.
- 29.4% asymmetry in isometric hamstring peak force (Hip Iso-Push), with absolute values that were poor on both limbs (injured: 1.2x SW, uninjured: 1.7x SW). Note: SW refers to the portion of body weight applied to the force plates – in this case, it is the weight support at the heel in the supine bridge position. For comparison, team sport males are expected to produce maximal force levels of at least 2-2.5x SW.
When presented with these objective testing results – what would you do?
In rehab, misjudging readiness to progress can lead to re-injury, loss of confidence and time lost. In this case, functional progress was evident, but capacity restoration was clearly lagging.
In rehab, misjudging readiness to progress can lead to re-injury, loss of confidence and time lost. In this case, functional progress was evident, but capacity restoration was clearly lagging.
This suggested that something else was likely going on, warranting further investigation. As Dan Pfaff puts it: “What else, where else?”
History Shapes Decision-Making: The ACL factor
The observed deficits were confounding, given the athlete’s functional abilities at that time. However, contextual injury history can be extremely important when interpreting the status of any athlete.
The observed deficits were confounding, given the athlete’s functional abilities at that time [but] injury history can be extremely important when interpreting the status of any athlete.
In this case, the athlete had previously undergone an ACLR on the affected limb using a hamstring graft (semitendinosus).
Persistent strength deficits in the hamstring complex are common following ACLRs with hamstring grafts. Given that the Nordic hamstring exercise primarily targets the semitendinosus, should we have expected the large asymmetry?
It is likely, but does that mean it should be ignored?
This is where decision-making becomes complex:
The answer to these questions lies somewhere in the middle. However, in this case, the strength deficits were too significant to ignore, but his functional status provided some confidence, which guided the next steps in his rehab.
Rehab Modifications and Training Adjustments
Based on these findings, my recommendation to the athlete and his support team was to:
1. Regress Running Intensity
Temporarily reduce running intensity, maintain sprinting at <80% maximal speed and avoid high-intensity accelerations and decelerations.
2. Reschedule His On-Field and In-Gym Rehab
As is often the case with sub-elite environments, athletes juggle work and sporting commitments. His weekly training structure was suboptimal for prioritizing force production development.
|
Monday
|
Tuesday
|
Wednesday
|
Thursday
|
Friday
|
Saturday
|
Sunday
| |
| AM |
|
|
|
|
|
On-field
|
|
| PM |
Lower body strength
|
On-field
|
|
On-field
|
Lower body strength
|
|
|
His prior training structure is outlined in the table above. The primary issue centered around recovery. The athlete’s main lower-body strength sessions (with hamstring stimulus) were occurring less than 24 hours prior to an upcoming on-field session. Thus, the athlete was either entering a strength session or an on-field session fatigued, reducing his ability to develop strength and speed.
Whilst important, he was structuring his weekly schedule to prioritize performing on-field sessions in a non-fatigued state. As a result, he deprioritized the restoration of underpinning strength qualities.
3. Emphasize Hamstring Strength Development
Prioritize maximal eccentric and isometric strength development across both proximally and distally dominant hamstring exercises. Several strategies were recommended:
- Increase the frequency of high-intensity eccentric exposures to two to three times per week.
- Implement one high-volume and high-intensity hamstring loading session per week.
|
Monday
|
Tuesday
|
Wednesday
|
Thursday
|
Friday
|
Saturday
|
Sunday
| |
| Theme |
Isometric (proximal) emphasis
|
On-field rehab
+ High-intensity eccentric exposure |
OFF LEGS
|
On-field rehab
|
Isometric (proximal) emphasis
|
On-field rehab
+ High-intensity, high-volume eccentric exposure |
OFF LEGS
|
| AM |
|
|
|
|
|
On-field
|
|
| PM |
Lower body strength
|
On-field
|
|
On-field
|
Lower body strength
|
|
|
| Suggested content and example exercises |
45° back extension Hamstring curls (isometric or isotonic) Hip bridge isometric hold (long duration) Single-leg hip thrust
|
Nordics post run (3-4 sets; move through a large range of motion via partner or band assistance)
|
|
Maximum velocity exposure emphasis (once strength improved)
|
Hip bridge isometric hold (long duration) Glute ham raise isometric hold (shorter holds and load)
|
Nordics (3-5 sets) Eccentric leg curl (2 up:1 down) Hip bridge isometric hold (3-5 sets x 3-5 reps [5-10s per rep])
|
|
Assessments Matter, but So Does Context
Although the athlete returned to play without re-injury at approximately 12 weeks post-injury, follow-up testing five months after the initial assessment indicated he still lacked confidence in maximal sprinting and acceleration.
At follow-up testing, two key assessments provided further insight:
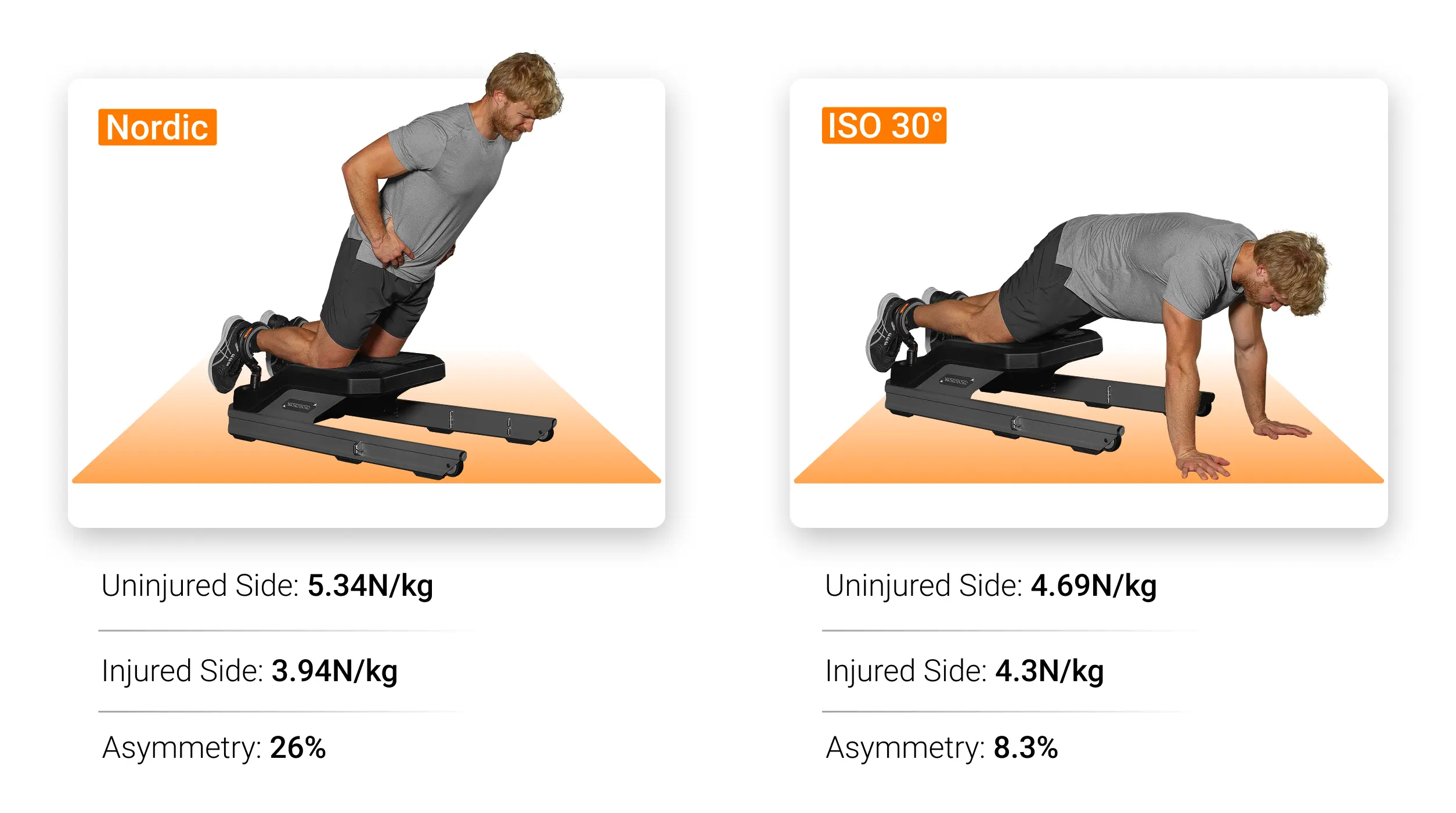
- Eccentric hamstring test (Nordic hamstring exercise) showed eccentric strength asymmetry remained persistent (somewhat expected) but had improved to 26%. This change resulted from a 46.3% strength increase on the injured side and a 28% improvement on the uninjured side. Absolute values improved significantly to 3.94N/kg on the injured side vs. 5.34N/kg on the uninjured side, placing the athlete in the 25th and 80th percentiles, according to the VALD 2021 Normative Data Report from Rugby Union. While progress was evident, symmetry was not achieved.
- Single-leg isometric hamstring test at 30° knee flexion (ISO 30) was introduced to further assess the biceps femoris given the persistent asymmetry. This assessment showed an 8.3% asymmetry, with absolute values within an acceptable range (4.3N/kg injured side vs. 4.69N/kg uninjured side).
This case highlights the risks of relying solely on a single test, as multiple overlapping assessments often provide necessary redundancy to help validate findings, confirm results and minimize errors.
Why does this matter? Asymmetries are often task-specific, and a single test can only tell so much.
Asymmetries are often task-specific, and a single test can only tell so much.
Had we relied solely on the Nordic test, we might have thought the athlete had a persistent deficit that placed him at risk. Although this was most likely due to the semitendinosus graft site from his previous ACL injury, it was clear that he still had a persistent deficit requiring consistent focus.
However, the additional assessment indicated that his biceps femoris strength, which was the likely injured site and a muscle critical for sprinting, was acceptably symmetrical and capable of producing good absolute force. Furthermore, bilateral assessments (such as the Nordic) allowed for greater opportunities to alter movement strategy to offload a particular limb (displaying greater levels of asymmetry), whereas the single-leg ISO 30 assessment offered a more precise measure of individual limb capacity.
This additional knowledge was therefore used as part of the decision-making processes, reinforcing the idea that assessment should not be binary. Rather than relying on pass/fail markers, which fail to capture the nuance of return-to-play readiness, assessment should be layered – considering how different tests interact with each other, as a milestone achieved in one area does not always indicate readiness in another.
…assessment should be layered – considering how different tests interact with each other…
Balancing Progression Against Function and Capacity
Decision-making in rehab and return-to-play situations is never an exact science. Should decision-making be based solely on functional abilities or should they ensure that underpinning capacities match functional demands? Both functional progression and isolated capacity assessment play integral roles during the return-to-play process, reinforcing the importance of balancing the two.
When selecting assessments, we require sufficient information to make informed decisions. Too many assessments introduce noise and additional complexity, while too few assessments can lead to blind spots, potentially missing critical deficits that increase re-injury risk.
Too many assessments introduce noise and additional complexity, while too few assessments can lead to blind spots, potentially missing critical deficits that increase re-injury risk.
It is also important not to forget that functional progression is an assessment in itself and should align with sport demands, athlete activities and tissue load. The following are important progression considerations during the reconditioning process:
- Use multiple overlapping assessments to confirm findings when needed.
- Ensure functional progression supports physical capacity restoration – if not, identify why.
- Continuously evaluate whether the athlete is progressing efficiently and effectively.
Ultimately, is the full picture being captured or just a fraction of it?
If you would like to learn how VALD’s human measurement technology can support your rehab decision-making by providing objective insights into hamstring strength, asymmetries and return-to-play progression, please reach out.
