Establishing Military Shoulder Strength Norms
Available in:
EN
In rehabilitation, setting specific, functional and standardized goals is critical to delivering quality outcomes. However, within specialist military populations, limited normative data for upper limb markers complicates return-to-work decisions, making such goal-setting difficult.
Joshua Ambler, BSc (Hons), GSR, set out to combat this issue, aiming to minimize the risk of reinjury and absenteeism in specialist military populations. He addressed these issues by establishing upper limb performance benchmarks using a database to support future clinical decision-making. This blog outlines his process and rationale for execution.
Background
Within a military population, common tasks like weapons handling, climbing, close-quarter battle (CQB) and resistance training require high levels of rotator cuff strength, scapulothoracic stability and global function for optimal performance in tactical populations.
…weapons handling, climbing, CQB and resistance training require high levels of rotator cuff strength…
While lower limb normative data exists for military populations, upper limb strength measures remain limited despite being well-documented in sporting contexts (Schwank et al., 2022; Cools et al., 2016; Borms & Cools, 2018).
Special forces team member on duty with current shoulder testing reports from VALD Hub.
Unlike sport, where physical preparation is geared toward peak performance in competition, military personnel must be ready to perform under fatigue at short notice. This reality underscores the need for individualized training programs tailored to functional demands and occupational standards.
Unlike sport…military personnel must be ready to perform under fatigue at short notice.
At the time of writing and collecting data, the Soldier Conditioning Review (SCR) serves as the primary assessment, comprising six tests:
- Broad jump
- Seated medicine ball throw
- Hex bar deadlift
- 100m shuttles
- Pull-ups
- 2km timed run

The six primary components of the SCR.
However, these tests act as proxy measures, where task completion or non-specific interval measures assume qualities like strength or power are present, rather than directly measuring them. Similarly, bilateral upper limb assessments further increase the risk of unidentified asymmetries, potentially elevating injury risk.
To maintain a healthy, operational military force, combat settings require precise, technology-informed assessments of individual limbs to identify injury risks, support individualized interventions and ensure consistent workforce readiness.
Assessment
A needs analysis highlights the broad skillset and demands required of military personnel. These often include:
- Parachuting
- Weapons handling
- Dog handling
- Breaching (explosive and physically enforced entry)
- Load carriage
These activities are often performed for long hours during extensive missions. It is, therefore, the duty of rehabilitation and performance personnel to go a step further and understand the underpinning qualities these tasks require, such as:
- Strength
- Power
- Agility
- Aerobic and anaerobic conditioning
- Cognitive processing
- Coordination
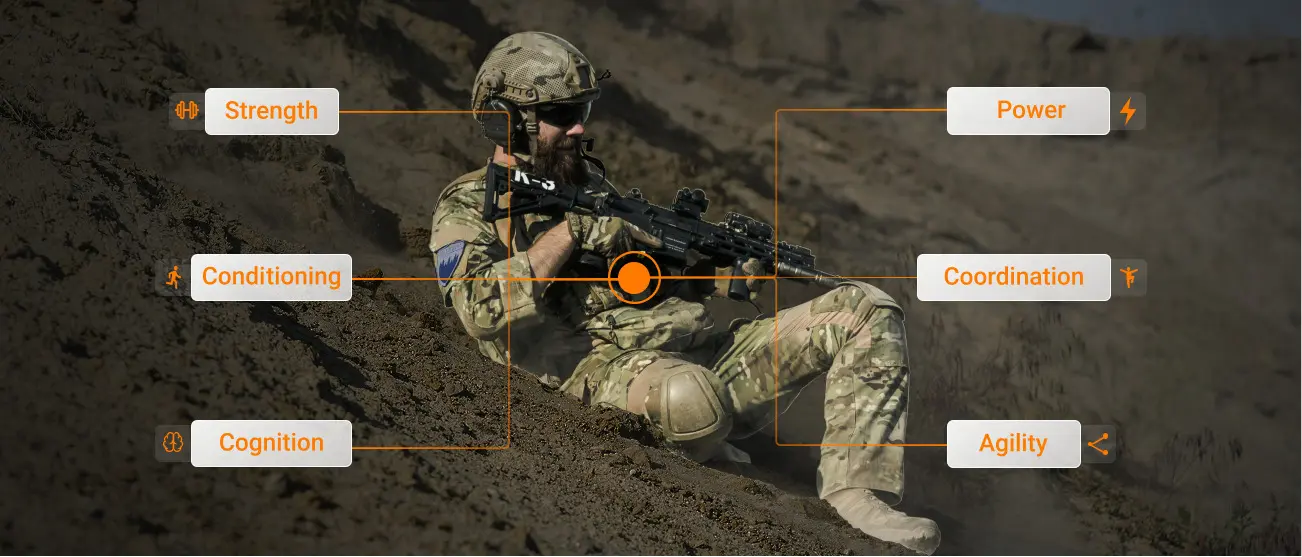
Underpinning characteristics assembled from a needs analysis of military personnel.
Unlike sport, the risks in this context go beyond injury and can extend as far as death, making physical readiness essential. As a result, attributes like maximal strength are strongly connected to performance, injury risk and even survival (Jochem et al., 2019; Suchomel et al., 2018).
…maximal strength [is] strongly connected to performance, injury risk and even survival.
Equally important is rate of force development (RFD). Research has highlighted RFD’s critical role in injury prevention, as exceeding tissue thresholds often leads to musculoskeletal injuries (Windt & Gabbett, 2017; Meeuwisse, 1994).
For the purpose of this article, shoulder external rotation (ER) and internal rotation (IR) assessments measured in the supine position at 90° of shoulder abduction and elbow flexion will be referred to as “ER/IR.”
To accurately assess shoulder strength in military populations, the project prioritized isometric testing using ForceFrame to measure shoulder ER/IR and ForceDecks to measure Athletic Shoulder (ASH) Test metrics. While isokinetic dynamometry (IKD) is considered the gold standard (van der Woude, 2022), its limited accessibility makes comparisons with U.S. Marine Special Forces data challenging (Poploski et al., 2018).
Furthermore, IKD often tests in neutral positions rather than the overhead or long-lever “at-risk” positions commonly encountered during military tasks. Shoulder ER/IR and the ASH Test (Ashworth et al., 2018) offer insights into glenohumeral joint and scapulothoracic stability when generating peak forces. Notably, the ASH Test assesses a soldier’s ability to stabilize the trunk against external forces, which is important for firing and maneuver drills.
The use of isometric assessments offers significant benefits, including lower risk, greater efficiency and true maximal force measurement (Lum & Barbosa, 2019). These assessments can be conducted more frequently without disrupting training cycles, providing consistent data for performance monitoring and injury risk mitigation.
…isometric assessments [are] low risk, [efficient] and…can be conducted more frequently without disrupting training…

Isometric shoulder assessment of on-duty military personnel.
Handheld dynamometry has limitations due to inter-rater reliability. However, when integrated into a fixed device like ForceFrame, reliability improves significantly, with intraclass correlation coefficient (ICC) values as high as 0.98 for shoulder ER/IR (Couch et al., 2021; Thorborg et al., 2013).
Normalizing strength data to body mass ensures fair comparisons across varied body sizes (Peterson et al., 2006). Using ForceDecks further enhances reliability, with ICC values up to 0.99 for the ASH Test across all metrics and positions (Collings et al., 2024).
Normalizing strength data to body mass ensures fair comparisons…[and] using ForceDecks further enhances reliability…
Normalized calculations are made simpler and faster with the Relative Strength Calculator on VALD's Calculators landing page.
Design
We created a database as a resource for assessing injured service personnel, with all protocols, documentation and data collection processes digitized for accessibility and sustainability. Standardized procedures were developed to ensure consistency, and staff received internal and external training from VALD to facilitate accurate data collection and database navigation.
Test selection focused on functional tasks relevant to the population and common upper limb injury markers, enabling retrospective analysis to guide future rehabilitation goals. Collected data included subject characteristics (injury status, age, weight, dominant limb, unit, etc.), injury dates and testing timelines. All data were anonymized using a patient-specific identification code, ensuring continuity across locations and assessors.
Test selection focused on functional tasks relevant to the population and common upper limb injury markers…
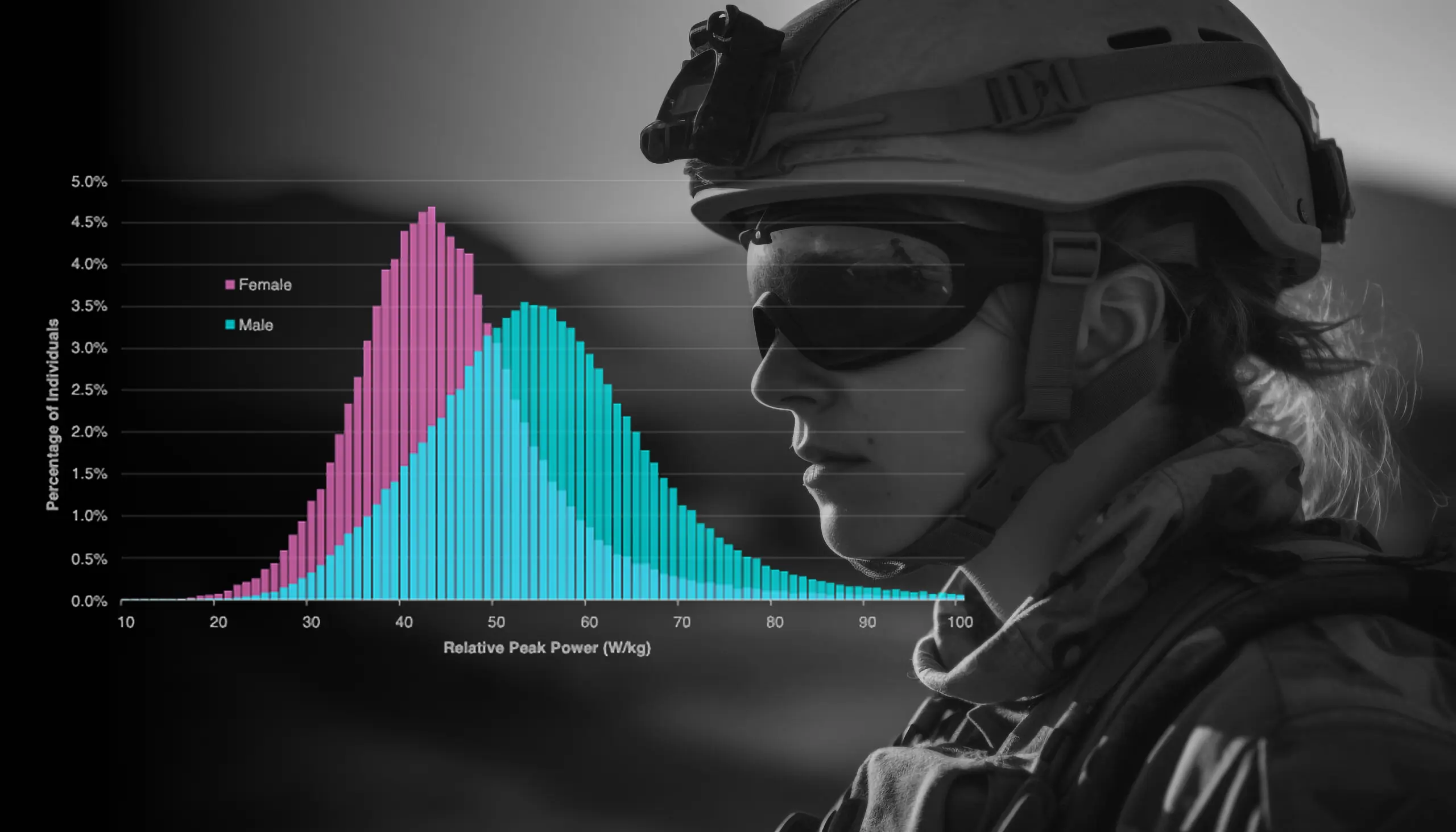
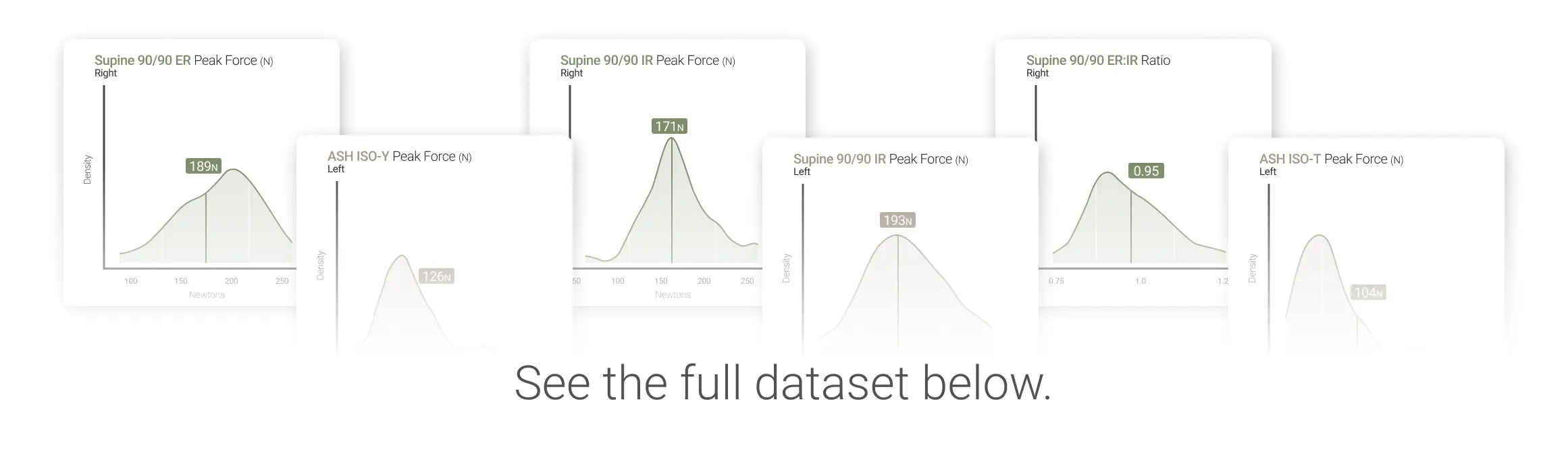
Normative data distributions for male and female military personnel.
Screening days involved groups of up to 20 individuals completing the ASH Test and ForceFrame ER/IR testing after consent, contraindication checks and optional physiotherapy appointments. Participants completed a warm-up, followed by three maximal trials per test, with additional trials if scores varied by more than 3%.
Peak force values were recorded and participants received personalized reports with recommendations for improving suboptimal scores, including exercise prescriptions and guidance to contact their Unit Physical Training Instructor (PTI) if further support was needed.
The normative benchmarking established through tests like the ASH Test and ForceFrame ER/IR testing enabled practitioners to identify outliers – those falling significantly above or below expected strength profiles for their role.
Notably, most soldiers tend to demonstrate adequate strength in the I position, but this is not always the case for the Y and T positions, where deficits are more common. These insights help guide individualized intervention plans, targeting specific weaknesses and informing rehabilitation, strength development or reconditioning efforts to ensure personnel are fully prepared for operational demands.
Results
ER/IR Testing
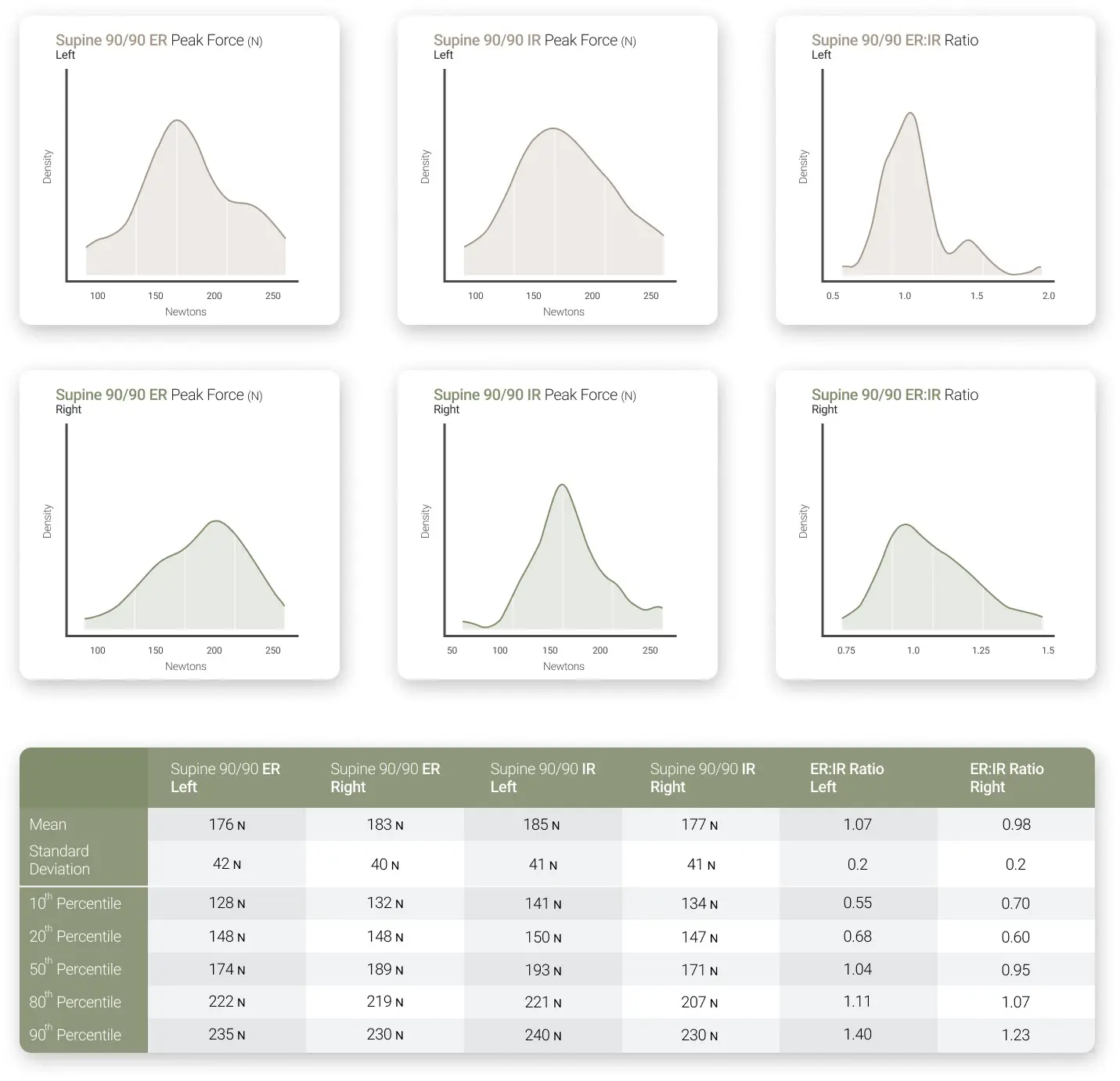
Normative data reports for shoulder ER/IR testing, provided by Joshua Ambler.
ASH Test
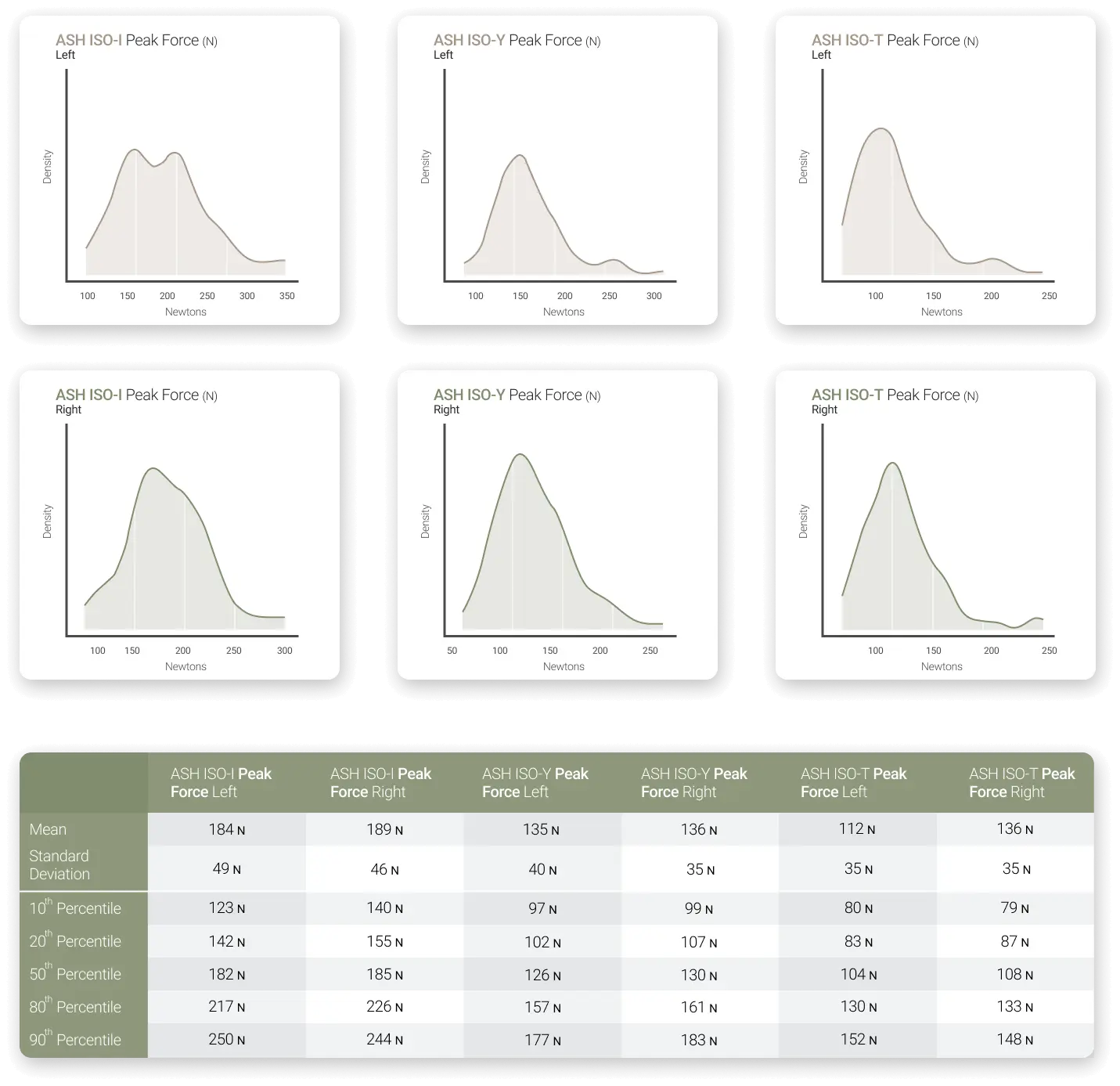
Normative data reports for the ASH Test, provided by Joshua Ambler.
Future Plans
At the time of drafting, the SCR was well established and up to date. However, as of April 1, 2025, the SCR will be modified to include a maximum-repetition push-up screening and to remove other assessments, such as the broad jump and seated medicine ball throw.
In response to these changes, this elite military unit will adapt its testing protocols to maintain comprehensive performance profiling. While continuing to use technology for assessment and rehabilitation, they will place greater emphasis on strength endurance metrics and leverage evolving data collection methods to refine return-to-duty decision-making.
The portability of VALD’s assessment technology makes in-field monitoring and assessments simple and easy to execute. Our ability to monitor and detect change extends and supports individuals’ time in a deployed role, optimizing their performance and our team’s effectiveness.
If you would like to learn more about integrating VALD’s human measurement technology into your organization to support upper limb testing, enhance return-to-duty decisions and reduce injury risk in specialist military populations, please reach out here.
References
- Schwank, A., Blazey, P., Asker, M., Møller, M., Hägglund, M., Gard, S., Skazalski, C., Haugsbø Andersson, S., Horsley, I., Whiteley, R., Cools, A. M., Bizzini, M., & Ardern, C. L. (2022). 2022 Bern consensus statement on shoulder injury prevention, rehabilitation, and return to sport for athletes at all participation levels. Journal of Orthopaedic & Sports Physical Therapy, 52(1), 11–28. https://www.jospt.org/doi/10.2519/jospt.2022.10952
- Cools, A. M., Vanderstukken, F., Vereecken, F., Duprez, M., Heyman, K., Goethals, N., & Johansson, F. (2016). Eccentric and isometric shoulder rotator cuff strength testing using a hand-held dynamometer: Reference values for overhead athletes. Knee Surgery, Sports Traumatology, Arthroscopy, 24(12), 3838–3847. https://doi.org/10.1007/s00167-015-3755-9
- Borms, D., & Cools, A. (2018). Upper-extremity functional performance tests: Reference values for overhead athletes. International Journal of Sports Medicine, 39(6), 433–441. https://doi.org/10.1055/a-0573-1388
- Jochem, C., Leitzmann, M., Volaklis, K., Aune, D., & Strasser, B. (2019). Association between muscular strength and mortality in clinical populations: A systematic review and meta-analysis. Journal of the American Medical Directors Association, 20(10), 1213–1223. https://doi.org/10.1016/j.jamda.2019.05.015
- Suchomel, T. J., Nimphius, S., Bellon, C. R., & Stone, M. H. (2018). The importance of muscular strength in athletic performance. Sports Medicine, 48(4), 765–785. https://doi.org/10.1007/s40279-018-0862-z
- Windt, J., & Gabbett, T. J. (2017). How do training and competition workloads relate to injury? The workload–injury aetiology model. British Journal of Sports Medicine, 51(5), 428–435. https://doi.org/10.1136/bjsports-2016-096040
- Meeuwisse, W. H. (1994). Assessing causation in sport injury: A multifactorial model. Clinical Journal of Sport Medicine, 4(3), 166–170. https://doi.org/10.1097/00042752-199407000-00004
- van der Woude, D. R., Ruyten, T., & Bartels, B. (2022). Reliability of muscle strength and muscle power assessments using isokinetic dynamometry in neuromuscular diseases: A systematic review. Physical Therapy, 102(10), pzac099. https://doi.org/10.1093/ptj/pzac099
- Poploski, K. M., Picha, K. J., Winters, J. D., Royer, S. D., Heebner, N. R., Lambert, B., Abt, J. P., & Lephart, S. M. (2018). Patterns and associations of shoulder motion, strength, and function in MARSOC personnel without history of shoulder injury. Military Medicine, 183(11-12), e685–e692. https://doi.org/10.1093/milmed/usy088
- Ashworth, B., Hogben, P., Singh, N., Tulloch, L., & Cohen, D. D. (2018). The athletic shoulder (ASH) test: Reliability of a novel upper body isometric strength test in elite rugby players. BMJ Open Sport & Exercise Medicine, 4(1), e000365. https://doi.org/10.1136/bmjsem-2018-000365
- Lum, D., & Barbosa, T. M. (2019). Brief review: Effects of isometric strength training on strength and dynamic performance. International Journal of Sports Medicine, 40(6), 363–375. https://doi.org/10.1055/a-0863-4539
- Couch, J., Sayers, M., & Pizzari, T. (2021). Reliability of the ForceFrame with and without a fixed upper-limb mold in shoulder rotation strength assessments compared with traditional hand-held dynamometry. Journal of Sport Rehabilitation, 30(8), 1246–1249. https://doi.org/10.1123/jsr.2020-0434
- Thorborg, K., Bandholm, T., Schick, M., Jensen, J., & Hölmich, P. (2013). Hip strength assessment using handheld dynamometry is subject to intertester bias when testers are of different sex and strength. Scandinavian Journal of Medicine & Science in Sports, 23(4), 487–493. https://doi.org/10.1111/j.1600-0838.2011.01405.x
- Peterson, M. D., Alvar, B. A., & Rhea, M. R. (2006). The contribution of maximal force production to explosive movement among young collegiate athletes. Journal of Strength and Conditioning Research, 20(4), 867–873. https://doi.org/10.1519/R-18695.1
- Collings, T. J., Lima, Y. L., Dutaillis, B., & Bourne, M. N. (2024). Concurrent validity and test–retest reliability of VALD ForceDecks strength, balance, and movement assessment tests. Journal of Science and Medicine in Sport, 27(8), 572–580. https://doi.org/10.1016/j.jsams.2024.04.014
